Recent Medical Discoveries in Blood: Understanding Blood Types, Their Mechanisms, and Evolutionary Significance
Blood, the life-sustaining fluid coursing through our veins, has been a subject of fascination and study for centuries. Recent advancements in medical science have deepened our understanding of blood, its types, and their evolutionary origins.
Recent Medical Discoveries in Blood
1. Discovery of New Blood Group Systems
In 2024, researchers identified a novel blood group system, the MAL blood group, which is defined by the presence or absence of the AnWj antigen. This discovery, published in Blood, resolved decades of mystery surrounding the AnWj antigen, previously known as a "ghost" antigen due to its elusive nature. The MAL blood group is significant for transfusion medicine, as individuals lacking the AnWj antigen can develop antibodies that complicate blood transfusions. This finding enhances the precision of blood matching, reducing the risk of transfusion reactions.
Additionally, advancements in genomics have led to the reclassification of existing blood group systems. For instance, the ER blood group, discovered in 2022, was further characterized in 2023, revealing its genetic basis in the PIEZO1 gene. These discoveries underscore the complexity of blood group systems beyond the well-known ABO and Rh systems, with over 40 recognized systems now documented.
2. Blood-Based Biomarkers for Disease Detection
Blood tests have become increasingly sophisticated, with recent studies highlighting their potential for early disease detection. In 2025, researchers developed a blood test capable of detecting Alzheimer’s disease up to 15 years before symptoms appear by measuring levels of p-tau217, a protein biomarker. This test, reported in Nature Medicine, achieves 97% accuracy and is being integrated into clinical practice in the UK.
Similarly, liquid biopsy techniques have advanced cancer detection. A 2024 study in The Lancet Oncology demonstrated that circulating tumor DNA (ctDNA) in blood can predict cancer recurrence with high sensitivity, enabling earlier interventions. These discoveries leverage blood’s role as a dynamic repository of biological information, revolutionizing diagnostics.
3. Advances in Artificial Blood and Blood Substitutes
The quest for artificial blood has gained momentum, with 2024 seeing breakthroughs in hemoglobin-based oxygen carriers (HBOCs). A study in Transfusion reported the development of a synthetic red blood cell substitute that mimics natural oxygen transport, showing promise in animal models. While not yet approved for human use, these substitutes could address blood shortages and provide alternatives for patients with rare blood types.
4. CRISPR and Blood Disorders
CRISPR gene-editing technology has transformed the treatment of blood disorders. In 2023, the FDA approved Casgevy, a CRISPR-based therapy for sickle cell disease and beta-thalassemia, which edits patients’ hematopoietic stem cells to produce functional hemoglobin. Clinical trials reported in New England Journal of Medicine showed that 95% of patients with sickle cell disease remained symptom-free two years post-treatment. This marks a significant milestone in curing genetic blood disorders.
Understanding Blood Types
What Are Blood Types?
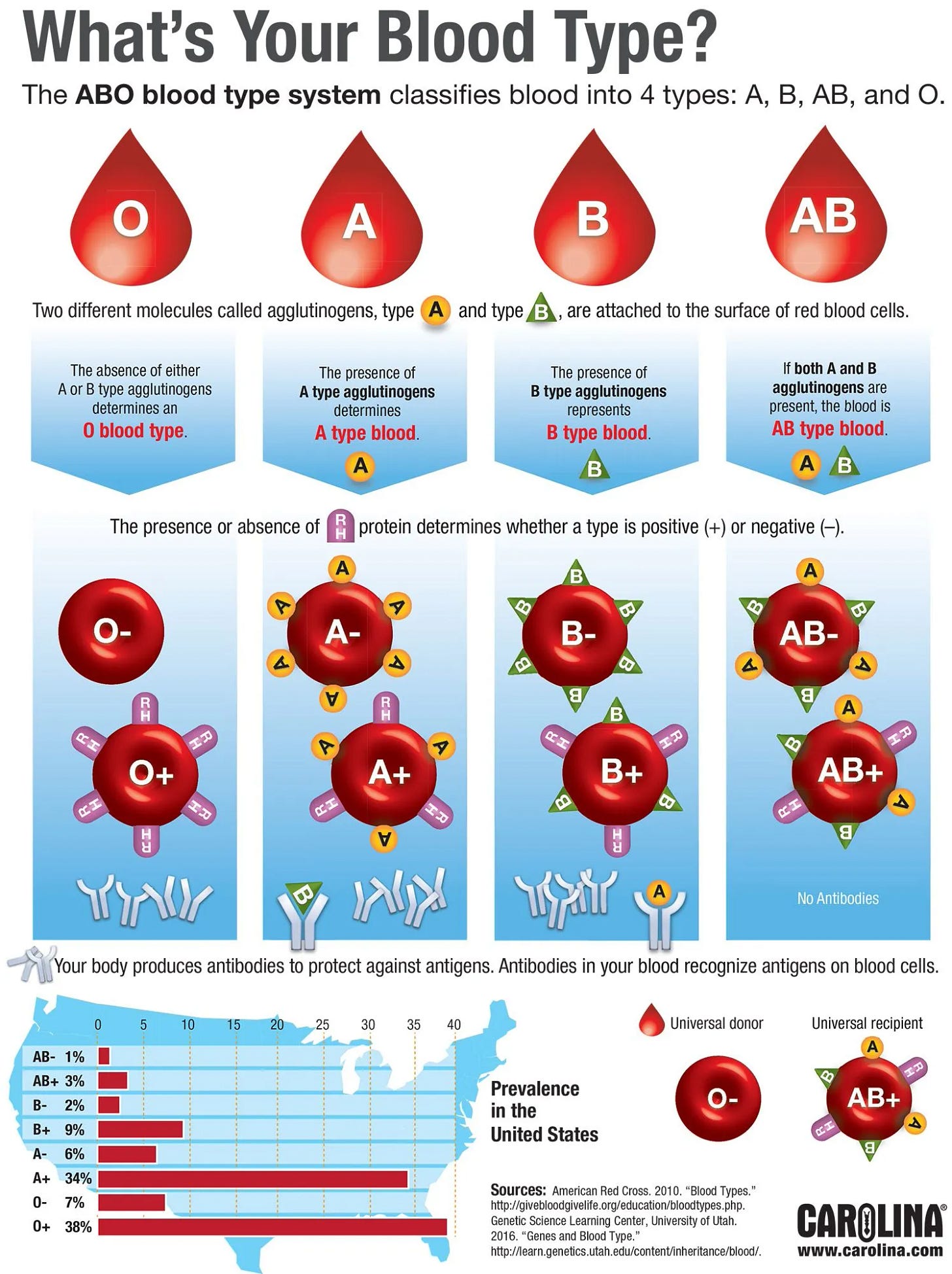
Blood types are classifications of blood based on the presence or absence of specific antigens—proteins or carbohydrates—on the surface of red blood cells. The two primary systems are:
-ABO System: Discovered by Karl Landsteiner in 1901, it categorizes blood into four types: A, B, AB, and O, based on A and B antigens. Type O lacks these antigens, making it the universal donor.
-Rh System: Identified in 1939, it determines whether blood is Rh-positive (with the D antigen) or Rh-negative (without it). This results in eight main blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-.
Other systems, like Kell, Duffy, and the newly discovered MAL, involve additional antigens that influence transfusion compatibility and disease susceptibility.
How Do Blood Types Work?
Blood types are determined by genetics, with genes encoding antigens inherited from parents. For example:
-ABO Genetics: The ABO gene on chromosome 9 has three alleles: A, B, and O. A and B are codominant, while O is recessive. A person with genotype AA or AO has type A blood; BB or BO yields type B; AB produces type AB; and OO results in type O.
-Rh Genetics: The RHD gene on chromosome 1 determines Rh status. A single functional copy results in Rh-positive blood, while two non-functional copies produce Rh-negative.
Antigens act as molecular “flags” recognized by the immune system. If a person receives incompatible blood (e.g., type A blood transfused into a type B individual), their immune system may attack the foreign antigens, causing potentially fatal hemolytic reactions. This is why blood typing and cross-matching are critical in transfusions.
Why Are There Different Blood Types?
The diversity of blood types is a product of evolutionary pressures, primarily driven by infectious diseases, environmental factors, and genetic drift. Each blood type may confer specific advantages or vulnerabilities:
-Type O: Common globally (around 43% of the population), type O may offer resistance to certain infections, like severe malaria caused by *Plasmodium falciparum*. The absence of A and B antigens reduces the parasite’s ability to bind to red blood cells.
-Type A: Linked to increased susceptibility to smallpox but may provide resistance to cholera. It’s prevalent in Europe and parts of Asia.
-Type B: Associated with resistance to some bacterial infections, like Escherichia coli, and is more common in Asia and Africa.
-Type AB: Rare (about 4% globally), it combines traits of A and B, potentially offering a balanced immune response but increasing risks for certain cancers.
-Rh-Negative: Found in about 15% of Europeans but rare elsewhere, Rh-negative blood may have evolved as a neutral mutation or in response to specific pathogens like Toxoplasma gondii.
Evolutionary Origins of Blood Types
Blood type diversity likely emerged millions of years ago in primate ancestors. The ABO system predates humans, with similar systems observed in chimpanzees and gorillas. Genetic studies suggest the A allele is the oldest, followed by B, with O arising later through mutations that inactivated the ABO gene.
Evolutionary theories propose:
1. Pathogen-Driven Selection: Blood group antigens interact with pathogens, influencing survival. For example, the Duffy antigen (part of the Duffy blood group system) serves as a receptor for Plasmodium vivax malaria. Duffy-negative individuals, common in West Africa, are resistant to this parasite, illustrating how blood types can evolve under disease pressure.
2. Diet and Environment: Some hypothesize that blood types correlate with dietary adaptations. Type A is linked to agricultural societies, while type O is associated with hunter-gatherer diets. However, this theory remains controversial due to limited genetic evidence.
3. Genetic Drift and Migration: As human populations migrated, founder effects and genetic drift shaped blood type distributions. For instance, the high prevalence of type B in Central Asia may reflect historical migrations of nomadic groups.
4. Reproductive Compatibility: Rh incompatibility, where an Rh-negative mother carries an Rh-positive fetus, can lead to hemolytic disease of the newborn. This suggests Rh-negative blood may have persisted despite reproductive disadvantages due to other survival benefits or genetic bottlenecks.
Why Blood Types Matter Today
Medical Implications
- Transfusions: Accurate blood typing prevents adverse reactions. The discovery of new blood groups like MAL improves matching precision.
- Pregnancy: Rh incompatibility is managed with RhoGAM injections to prevent maternal-fetal complications.
- Disease Susceptibility: Blood types influence disease risk. Type O individuals have a lower risk of severe COVID-19 outcomes, while type A is linked to higher susceptibility, per a 2023 study in Blood Advances.
Societal Impact
Blood type shortages, particularly for rare types like AB- or Rh-negative, highlight the need for diverse donor pools. Innovations like artificial blood and gene-editing therapies aim to address these challenges, while public health campaigns emphasize the importance of blood donation.
Future Directions
The future of blood research is promising, with ongoing studies exploring:
-Personalized Medicine: Blood-based biomarkers could guide tailored treatments for cancer, Alzheimer’s, and cardiovascular diseases.
-Universal Blood: Scientists are developing methods to enzymatically remove A and B antigens from red blood cells, creating universal donor blood.
-Synthetic Biology: Advances in lab-grown blood, such as red blood cells cultured from stem cells, could revolutionize transfusion medicine.
Recent discoveries in blood science, from new blood group systems to gene-editing therapies, underscore the complexity and vitality of this field. Blood types, shaped by millions of years of evolution, reflect humanity’s adaptation to diverse environments and pathogens.
Understanding their mechanisms not only enhances medical practice but also illuminates our shared history. As research progresses, blood will continue to unlock secrets to health, disease, and human survival, ensuring its place at the heart of medical innovation.